
[ad_1]
OAKLAND, Calif. — Medi-Cal well being protection kicked in for Antonio Abundis simply when the custodian wanted it most.
Shortly after Abundis transitioned from restricted to full-scope protection in 2022 beneath California’s enlargement of Medi-Cal to older residents with out authorized immigration standing, he was recognized with leukemia, a most cancers affecting the blood cells. The soft-spoken father of three took the information in stride as his physician mentioned his blood take a look at advised his most cancers wasn’t superior. His subsequent steps had been to get extra assessments and formulate a remedy plan with a most cancers crew at Epic Care in Emeryville. However all of that was derailed when he confirmed up final July for bloodwork at La Clínica de La Raza in Oakland and was informed he was now not on Medi-Cal.
“They by no means despatched me a letter or something telling me that I used to be eliminated,” Abundis, now 63, mentioned in Spanish about shedding his insurance coverage.
Abundis is amongst a whole lot of hundreds of Latinos who’ve been kicked off Medi-Cal, California’s Medicaid program for low-income individuals, as states resume annual eligibility checks that had been paused on the peak of the covid-19 pandemic. The redetermination course of, as it’s identified, has disproportionately affected Latinos, who make up a majority of Medi-Cal beneficiaries. Based on the California Division of Well being Care Providers, greater than 653,000 of the greater than 1.3 million residents who’ve been disenrolled over eight months determine as Latino. Some, together with Abundis, had solely lately gained protection because the state expanded Medi-Cal to residents with out authorized residency.
The collision of state and federal insurance policies has not solely set off enrollee whiplash however swelled demand for enrollment help as persons are dropped from Medi-Cal, typically for procedural points. Well being teams serving Latino communities report being inundated by requests for assist, however on the identical time, a state-sponsored survey suggests Hispanic households are extra doubtless than different ethnic or racial teams to lose protection as a result of they’re much less educated of the renewal course of. They could additionally wrestle to advocate for themselves.

Some well being advocates are urgent for a pause. They warn that disenrollments won’t solely undercut the state’s effort to cut back the variety of uninsured however might exacerbate well being disparities, significantly for an ethnic group that bore the brunt of the pandemic. One nationwide research discovered that Latinos within the U.S. had been 3 times as more likely to contract covid and twice as more likely to die of it than the final inhabitants, partially as a result of they have a tendency to stay in additional crowded or multigenerational households and work in front-line jobs.
“These difficulties place all of us as a group on this extra fragile state the place the protection internet means much more now,” mentioned Seciah Aquino, government director of the Latino Coalition for a Wholesome California, a well being advocacy group.
Meeting member Tasha Boerner, an Encinitas Democrat, has launched a invoice that may gradual disenrollments by permitting individuals 19 and older to maintain their protection routinely for 12 months and lengthen versatile pandemic-era insurance policies akin to not requiring proof of earnings in sure circumstances for renewals. That will profit Hispanics, who make up almost 51% of the Medi-Cal inhabitants in contrast with 40% of the general state inhabitants. The governor’s workplace mentioned it doesn’t touch upon pending laws.
Tony Cava, a spokesperson for the Division of Well being Care Providers, mentioned in an electronic mail that the company has taken steps to extend the variety of individuals routinely reenrolled in Medi-Cal and doesn’t contemplate a pause needed. The disenrollment fee dropped 10% from November to December, Cava mentioned.
Nonetheless, state officers acknowledge extra could possibly be finished to assist individuals full their purposes. “We’re nonetheless not reaching sure pockets,” mentioned Yingjia Huang, assistant deputy director of well being care advantages and eligibility at DHCS.
California was the first state to broaden Medicaid eligibility to all certified immigrants no matter authorized standing, phasing it in over a number of years: kids in 2016, younger adults ages 19-26 in 2020, individuals 50 and older in 2022, and all remaining adults this 12 months.
However California, like different states, resumed eligibility checks final April, and the method is predicted to proceed by Could. The state is now seeing disenrollment charges return to pre-pandemic ranges, or 19%-20% of the Medi-Cal inhabitants annually, in response to DHCS.
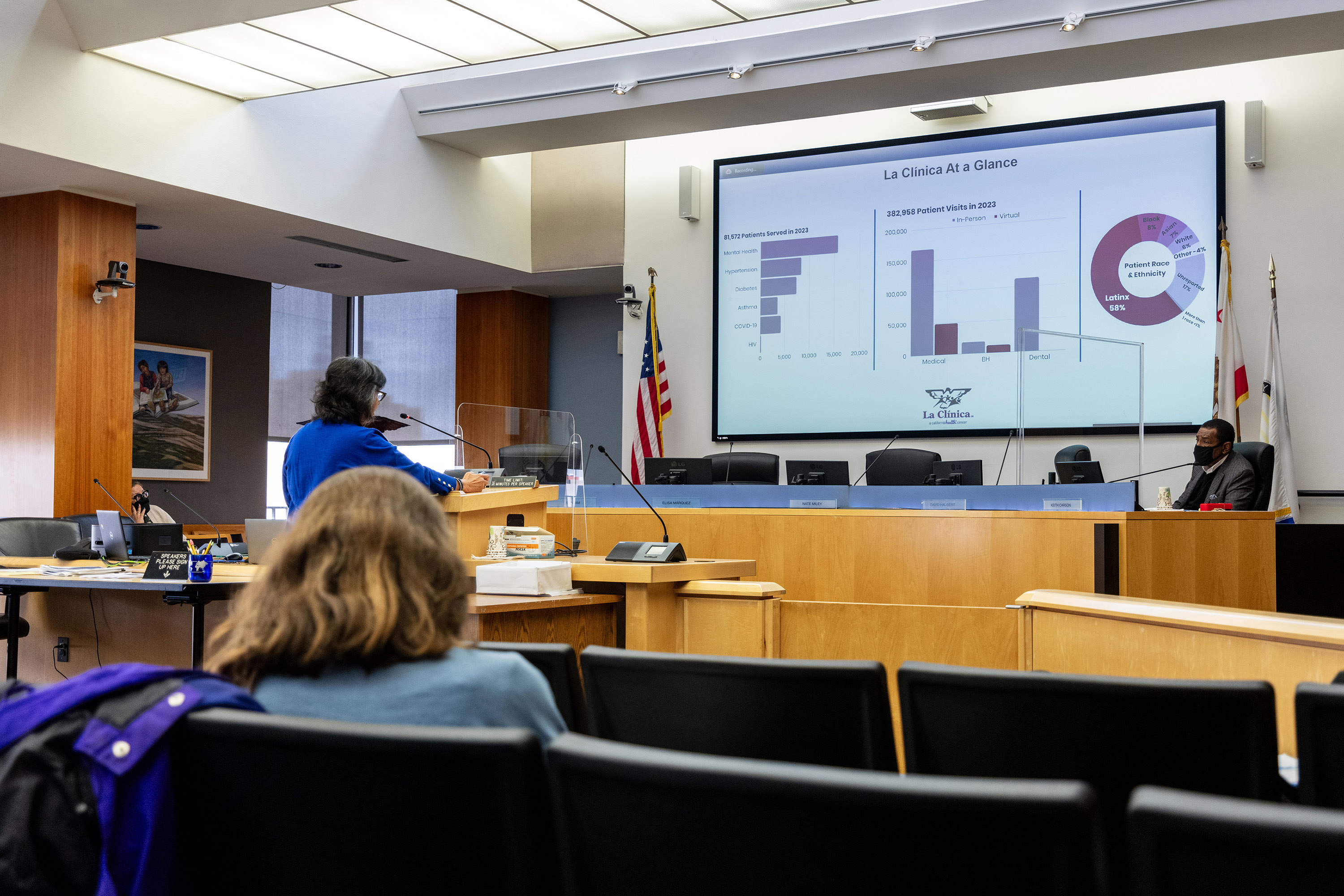
Jane Garcia, CEO of La Clínica de La Raza, testified earlier than the Alameda County Board of Supervisors’ well being committee that disenrollments proceed to pose a problem simply as her crew tries to enroll newly eligible residents. “It’s a heck of a load on our workers,” she informed supervisors in January.

Though many beneficiaries now not qualify as a result of their incomes rose, extra have been dropped from the rolls for failing to reply to notices or return paperwork. Usually, renewal packets had been despatched to previous addresses. Many discover out they’ve misplaced protection solely upon in search of medical care.
“They knew one thing was taking place,” mentioned Janet Anwar, eligibility supervisor at Tiburcio Vasquez Well being Heart within the East Bay. “They didn’t know precisely what it was, the way it was gonna have an effect on them till really the day got here they usually had been disenrolled. And so they had been getting checked in or scheduling an appointment, then, ‘Hey, you misplaced your protection.’”
However reenrollment is a problem. A state-sponsored survey printed Feb. 12 by the California Well being Care Basis discovered 30% of Hispanic households tried however had been unable to finish a renewal type, in contrast with 19% for white non-Hispanic households. And 43% of Hispanics reported they want to restart Medi-Cal however didn’t know the way, versus 32% of individuals in white non-Hispanic households.
The Abundis household is amongst those that don’t know the place to get their questions answered. Although Abundis’ spouse submitted the household’s Medi-Cal renewal paperwork in October, his spouse and two kids who nonetheless stay with them had been in a position to keep protection; Abundis was the one one dropped. He hasn’t acquired a proof for being disenrolled nor been notified the best way to attraction or reapply. Now he worries he could not qualify on his personal primarily based on his roughly $36,000 annual earnings because the restrict is $20,121 for a person however $41,400 for a household of 4.
It’s doubtless an eligibility employee might verify if he and his household qualify as a family or help him with signing up for a non-public plan that may run lower than $10 a month for premiums on Coated California. The medical insurance trade permits for particular enrollment when individuals lose Medi-Cal or employer-based protection. However Abundis assumes he gained’t be capable of afford premiums or copays, so he hasn’t utilized.
Abundis, who first visited a physician in Could 2022 about unrelenting fatigue, fixed ache in his again and knees, shortness of breath, and unexplained weight reduction, worries he’s unable to afford medical care. La Clínica de La Raza, the group well being clinic the place he acquired blood testing, labored with him that day so he didn’t should pay upfront, however he has since stopped in search of medical care.
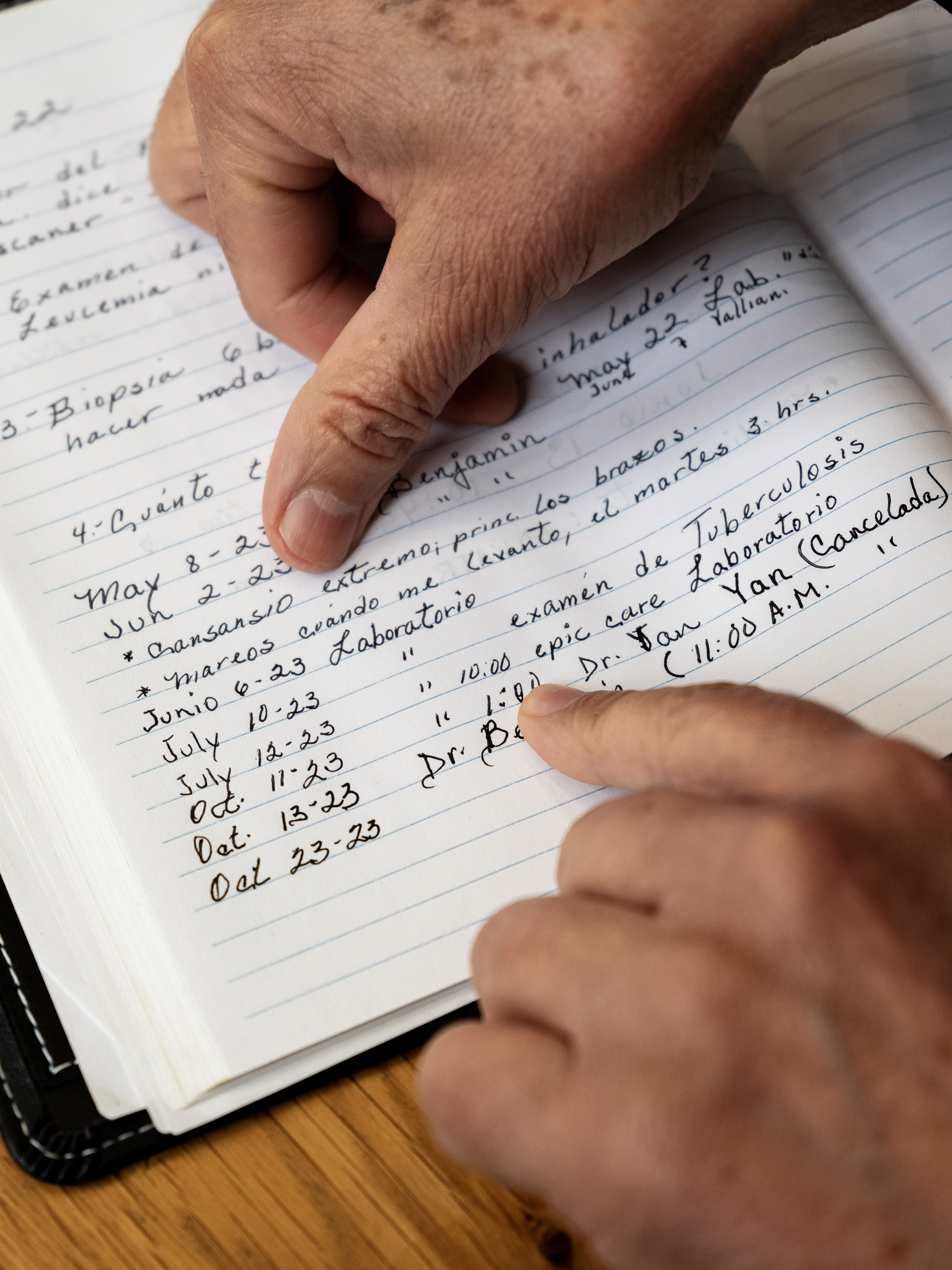
Greater than a 12 months after his analysis, Abundis nonetheless doesn’t know which stage most cancers he has, or what his remedy plan needs to be. Although early most cancers detection can result in a larger likelihood of survival, some varieties of leukemia advance shortly. With out additional testing, Abundis doesn’t know his outlook.
“I’ve mentally ready,” Abundis mentioned of his most cancers. “What occurs, occurs.”
Even those that search assist run into challenges. Marisol, a 53-year-old immigrant from Mexico who lives in Richmond, California, with out authorized permission, tried to reestablish protection for months. Though the state noticed a 26% drop in disenrollments from December to January, the share of Latinos disenrolled throughout that interval remained almost the identical, suggesting they face extra obstacles to renewal.
Marisol, who requested her final title be withheld out of concern of deportation, additionally certified for full-scope Medi-Cal through the state enlargement to all immigrants 50 and older.
She acquired a packet in December letting her know that her family earnings exceeded Medi-Cal’s threshold — one thing she believed was an error. Marisol’s husband is out of labor on account of a again damage, she mentioned, and her two kids primarily assist their household with part-time jobs at Ross Gown for Much less.
That month, Marisol visited a Richmond department workplace of the Contra Costa County Employment and Human Providers Division, hoping to talk to an eligibility employee. As an alternative, she was informed to go away her paperwork and to name a telephone quantity to verify her software standing. Since then, she made quite a few calls and spent hours on maintain, however has not been in a position to communicate with anybody.
County officers acknowledged longer wait occasions on account of elevated calls and mentioned the common wait time is half-hour. “We perceive group members’ frustration once they have issue getting by at occasions,” spokesperson Tish Gallegos wrote in an electronic mail. Gallegos famous the decision middle will increase staffing throughout peak hours.
After El Tímpano reached out to the county for remark, Marisol mentioned she was contacted by an eligibility employee, who defined that her household was dropped as a result of their kids had filed taxes individually, so the Medi-Cal system decided their eligibility individually slightly than as one family. The county reinstated Marisol and her household on March 15.
Marisol mentioned regaining Medi-Cal was a joyous however bittersweet ending to a months-long wrestle, particularly realizing that different individuals get dropped for procedural points. “Sadly, there needs to be strain for them to repair one thing,” she mentioned.
Jasmine Aguilera of El Tímpano is collaborating within the Journalism & Girls Symposium’s Well being Journalism Fellowship, supported by The Commonwealth Fund. Vanessa Flores, Katherine Nagasawa, and Hiram Alejandro Durán of El Tímpano contributed to this text.
Medi-Cal Sources (in Spanish):
Find out how to apply for Medi-Cal
Find out how to get insurance coverage and low-cost well being care in California
Find out how to apply for Coated California
This text was produced by KFF Well being Information, which publishes California Healthline, an editorially impartial service of the California Well being Care Basis.
[ad_2]